Translate this page into:
Surgery for early stage endometrial carcinoma in the obese patient
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Obese patients have increased risk of developing endometrial cancer proportional to the excess in body mass index. In this review, we explored the latest information on surgical management and its adaptation to the obese condition. Mini-invasive treatments (laparoscopic, robotic, vaginal, or combinations) should be systematically considered. Prevention and active treatment of obesity seem an interesting approach to reduce incidence and severity of the disease.
Keywords
Body mass index
endometrial cancer
sentinel node
Introduction
Endometrial cancer (EC) is the fifth cause of feminine cancer in Europe, but the second gynecologic cancer worldwide. Thanks to an early patient’s detection by postmenopausal vaginal bleeding, its prognosis is rather good with a global rate of 70% 5-year survival (which can rise to 95% in International Federation of Gynecology and Obstetrics [FIGO] stage 1 well-differentiated endometrioid tumors).1 However, this tumor usually occurs in aged patients, presenting comorbidities. This explains the important fact that 50% of EC patients die from a non-EC-related cause.2 In this review, we focused on the obese population and therapeutic options, especially for early stage disease.
Epidemiological Data
90–95% of endometrial tumors are of epithelial subtype, the others 5–10% consisting of sarcomas.3 It is clearly accepted that these carcinomas can be shared in two distinct histopronostic subtypes4 with specific epidemiologies. Type 1 carcinomas are of the endometrioid subtype. They are the most frequent and are of a good global prognosis. These tumors are linked to any situations of relative hyperestrogenism which stimulates endometrium development, unbalanced by an adequate progesterone secretion. Apart from rare iatrogenic situations,5 hyperestrogenism is usually endogenic. It is observed in post- or peri-menopausal patients, often nulli- or pauci-parous, with a long life (early menses, late menopause) of ovulations.6 The polycystic ovarian syndrome7 is related to this condition of aborted ovulations. Obesity acts as a powerful cofactor of hyperestrogenism and consequently, is a strong factor favoring disease development and its related mortality.8
Type 2 EC encompass all nonendometrioid carcinomas such as serous, clear cell, or undifferentiated carcinomas and carcinosarcomas. Of much poorer prognosis than type 1 tumors, they are not clearly related to a specific etiological condition, except for tamoxifen use which may favor the development of this tumor subtype.9
In addition, 2–5% of EC are related to mismatch repair (MMR) system deficiency syndrome, as observed in the hereditary Lynch syndrome.10 It affects women at a younger age for the pathology, and MMR abnormality should be systematically sought in the tumor of these patients by immunohistochemistry since they are at a higher risk of other future malignancies (colon, kidney, bladder, or breast).11 Of interest is the fact that both type 1 (especially high grade) or 2 carcinomas have been reported in this context at a relative equal incidence.12
Recently, genomic studies provide, besides the pathological classification, a new molecular classification of ECs with four specific prognostic signatures that may impact future personalized management of this disease.3
Obesity is thus an important factor for the development of EC. The World Health Organization definition of obesity is clear and is based on body mass index measurements (BMI = weight [kg]/height [m2]). Obesity starts at a BMI ≥30.13
Obesity is observed worldwide with a great discrepancy according to socioeconomic level and activity of the population. Thus, obesity affects especially some islands, at first rank Nauru and Samoa islands, with 75% of population with mean BMI >30, 34% in the USA and 20–25% for Europe and <1% in Vietnam, India or Japan.13 More worrying, is the general soaring of obesity, especially in some unexpected countries such as Australia (+81%), New Zealand +93%, even India (+33%)! Even in France, 20% of population is obese, with an increase by 42% in 30 years.14
Apart from EC, obesity is responsible, through hormone imbalance and/or local inflammation, of other malignancies such as breast, ovary, colorectal, biliopancreatic, and even esophageal carcinomas!15 Specific biological mechanisms at the origin of EC development are complex and, for type 1 EC, involve both a relative hyperestrogenism status through conversion of circulating androgens into estrogens in adipocytes, not compensated by a progesterone secretion and a chronic inflammatory process through cytokines secretion.16 Other factors may favor the development of type 1 endometrial tumors such as type 2 diabetes mellitus or arterial hypertension, possible consequences of obesity as well. This explains why, although not exclusive, low-grade type 1 tumors are more frequently observed in the obese population than high-grade type 1 or 2 carcinomas,17 and at earlier stages. However, recent studies confirm that type 2 tumors are observed as well in an obese patient making their mechanism more complex than expected.18
Hysterectomy in Obese Early Endometrial Cancer Patients
The current management of EC is based on surgery that enables tumor removal and staging.
As recommended by the most international guidelines, early stage EC needs, at least, a total hysterectomy, and bilateral salpingo-oophorectomy (TH-BSO). Pelvic and paraaortic node dissection are discussed in tumors with intermediate or high risk of recurrence and in type 2 tumors.
Even in higher stage, surgery should be the first option to exercise before any other treatment such as radiation therapy, chemo and/or hormone therapies, which are usually employed as adjuvant treatments or definitively in inoperable patients.19
A total extrafascial hysterectomy without vaginal cuff is to be performed. Subtotal hysterectomy is never indicated in EC due to the not rare occult epithelial or stromal cervical involvement and may require implies secondary trachelectomy. The indication for radical hysterectomy is quite infrequent, even in case of overt cervical involvement since it does not impact survival.20
Except in very young patients for whom fertility preservation management may be considered, BSO is systematically recommended. Indeed, EC patients are at peri- or post-menopausal age, the risk of occult ovarian metastasis is significant (6.7% for Fadare),21 as well as the risk of adnexal carcinomas.
The route to perform this operation, laparotomy, laparoscopy, vaginal approach, has been for long a matter of debate.
Thanks to the results of several randomized trials and meta-analysis,22 the situation is clearer. Laparoscopic surgery is clearly the method of choice to perform the surgical treatment and staging of early EC. Besides cosmetic advantages, the absence of laparotomy significantly reduces perioperative morbidity, length of hospital stay, and enables a quick recovery and return to previous activities.
To perform a TH-BSO, the issue of a full laparoscopic or a laparoscopically-assisted vaginal technique has been addressed in a small-size randomized study. Surgical outcomes were similar in both groups, but obese patients benefitted of a shorter operative time with the full laparoscopic approach.23
Indeed, for obese and more for morbidly obese (BMI ≥40) patients, avoiding laparotomy, thanks to a mini-invasive approach (laparoscopic or vaginal route), is always an advantage, as shown in a recent systematic review of the literature in obese EC patients (Blikkendaal et al. AGO 2015).24
However, the adequate oncologic management of EC is not always feasible in obese or morbidly obese patients, because of the obesity itself and patient’s comorbidities. In the largest LAP2 randomized trial that compared open to laparoscopic management of early EC, 26% of patients in the laparoscopy arm had be converted into laparotomy because of obesity. Indeed, the requested pelvic and paraaortic lymphadenectomies could not be performed safely by all surgeons.
A good experience in laparoscopic surgery is required to manage obese patients. This experience is not restricted to the surgeon but concerns all the operative team. Nurses must be aware of a correct installation of the patient on the table. The anesthesiologists are especially concerned by these heavy patients often fragilized due to their comorbidities. Indeed, a prolonged high abdominal pressure due to both gas distension and Trendelenburg positioning may deeply affect ventilation and surgical tolerance. When all these conditions are fulfilled the rate of success of laparoscopic management is pretty high even in morbidly obese patients.25
For surgeons, the main problem is the correct visualization of the operative field. The ports may sometimes be placed higher on the abdomen, above the umbilicus, especially for the optique. Then, a good pelvis exposure needs a sufficient and progressive Trendelenburg positioning, “negotiated” with the anesthesiologist.
A clear view of the pelvis may need additional bowel retraction thanks to transparietal suspensions, using sutures or disposable devices adapted to obese patients (T-lift® – Vectec France).
For dissections, the adequate use of integrated sealing-cutting instruments (Ligasure®-Covidien, Ultracision®-Ethicon, Thunderbeat®-Olympus…) will facilitate the operation and shorten its duration.
In case of a large uterus, the preventive coagulation/clipping of uterine arteries at their origin will reduce blood loss (Roman et al. JSLB 2008).26 In-the-field specimen morcellation is strictly forbidden to prevent tumor spread. Placement of uterine specimen in an adapted and strong endoscopic bag will enable the vaginal extraction and if necessary the in-a-bag hemisection of the enlarged specimen27 Figure 1.
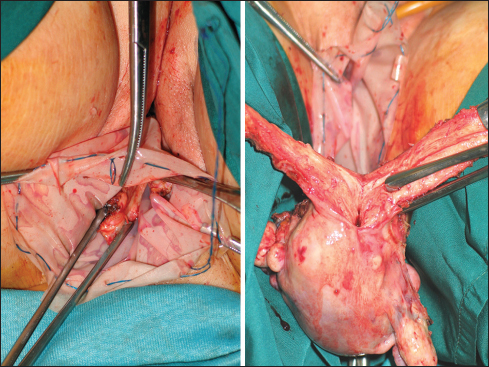
- In-a-bag (Lapsac®-Cook medical) specimen hemisection
However, in some extreme situations (morbid obesity, history of laparotomies), laparoscopic surgery cannot be performed or tolerated. Except if obvious contraindication (abdominal spread, inadequacy between uterus size [on preoperative magnetic resonance imaging]28 and the vaginal access), an exclusive vaginal approach should be attempted, before convert into laparotomy, especially in elderly patients.29 As for laparoscopy, the use of integrated instruments makes this approach easier to complete. If BSO cannot be performed vaginally, the installation of a single port system will make this step easier to complete the operation laparoscopically through the vagina!
Lymph Node Dissections of Endometrial Cancer in Obese Patients
The most challenging problem in obese EC patients is the completion of the staging procedures.
Fortunately, the results of recent randomized trials and meta-analysis are helpful, since lymph node dissections do not improve survival rates but increase morbidity, especially in early stage low-grade EC30 (…which is the most frequent situations in obese or morbidly obese patients!). However, they remain indicated in case of higher stage or grade disease. Technically, when pelvis is adequately exposed, a latero iliac approach of the paravesical spaces is often easier to complete a pelvic node dissection, than the classical medial approach. In the future, it is likely that, in normal-appearing pelvic node basins, the sentinel node (SN) dissection may replace full pelvic lymphadenectomies, as shown in prospective nonrandomized studies. However, some technical aspects must be standardized, such as the technique of tracer injection and the best tracer to use. Deep and superficial intracervical injections at 3 and 9 O’clock in the cervix, although criticized since the method detects the uterus SN, rather than specific to tumor. This recurrent criticism is similar to the same issue concerning SN in breast cancer for which the intradermal injection of tracer provided same results as deep peritumoral injections.31 Furthermore, the hysteroscopic tracer injections are technically more complex to perform and are especially challenging in case of large intracavitary tumors. Thus, intracervical injections seem the easiest and most efficient method to use as a routine, with the highest detection rates even if paraaortic SN are less frequently observed.32 Some results of prospective studies of SN in EC show lower detection rates compared SN in cervix cancer.33,34 However, the regular use of the “algorithm” (site specific full dissection in the absence of SN detection) reduces the risk of false negative of the method to <5%, thus detection rates are equivalent to results in cervix cancer.35,36
Concerning the tracers, recent studies assessing indocyanine green (ICG) and near-infrared (NIR) light detection report detection rates similar to radiotracer and superior to any kind of blue dye.37 The advantages of this technology are simplification of patient’s management (no need of preoperative injections of radiocolloid followed by scintigraphies) and prevention of useless irradiation. High BMIs do not impair detection rates, but bilateral detection rate seem higher when using combination of ICG and NIR light detection.38 However, the promising results of this policy deserve to be confirmed in larger prospective cohorts or a randomized studies.
When paraaortic dissection is requested in EC, it should be performed bilaterally, and up to the left renal vein.39 To complete this procedure laparoscopically is really challenging in obese EC and is with uterus size, FIGO stage, one of the major reasons for conversion into laparotomy with increased morbidity.40 Indeed, the transperitoneal approach is sometimes very challenging due to the thickness and shortness of mesentery. The extraperitoneal laparoscopic paraaortic approach as described by Dargent et al.41 may compensate, until some level, the difficulties of the transperitoneal approach and provides higher node counts even in higher BMIs, as highlighted in a recent comparative study of these two laparoscopic approaches (Pakish et al. GO 2014).42
The Robotic Approach
The robotic approach has been claimed to facilitate the global management of obese patients whatever the indication, thanks to the mechanical elevation of the abdominal wall that enable to decrease abdominal gas pressure. In Seamon’s paper, it was shown that the rate of conversion to laparotomy was delayed for higher BMI when compared to laparoscopy (Seamon et al. GO 2009).43
However, it must be stressed that a real experience in robotic surgery is mandatory to safely complete this operation in a reasonable operative time. Even in expert teams using the robot, the infrarenal paraaortic dissection is feasible in only 70% of obese compared to 88% in non-obese EC patients.44
Finally, the choice of minimally-invasive techniques in morbidly obese patients result in longer operative times but lower rates of blood loss and shorter hospital stays compared to laparotomy, and should be preferred.45 Compared to laparoscopic approach, robotic surgeries provide comparable complication rates but charges are higher.46
Nonsurgical Management of Early Stage
But even the best surgeons have know limits! In approximately, 10% of patients, extremely obese with an early stage EC along with life-threatening comorbidities (cardiovascular disease, organ failure due to diabetes mellitus, ventilation difficulties), general anesthesia is contraindicated or even mini-invasive surgery is not tolerated. In these situations, other alternative treatments must be considered. In a recent series of 43 high-operative risk patients with a FIGO I–III EC, the management consisted of definitive radiation therapy, encompassing external beam radiation therapy and high-dose rate intracavitary brachytherapy. 4.9% grade 3 toxicities were reported. With a median follow-up of 29 months, 8.3% local recurrences and 13% distal recurrences (restricted to grade 3 diseases) were observed with 2-year survival rate of 65%.47
Prevention
Finally, although the adequate use of minimally invasive surgery has increased success rates of the surgical treatment of ECs in obese patients, the best policy is to prevent obesity by a well-balanced diet along with physical activity. It has been demonstrated that treatments of obesity strongly reduce the incidence of EC as well as several other malignancies48 and related cardiovascular mortality.49 early type 1 or atypical hyperplasia.
Recently, bariatric surgery has demonstrated its efficacy in reducing both the incidence of this disease by more than 70% as well as its recurrence risk!50 possibly thanks to the reduction of estrogen receptor expression.51
Conclusions
Given its multiple advantages in terms of perioperative outcomes with no impairment of oncological results, minimally-invasive surgery (laparoscopy with or without robotic assistance or vaginal surgery) should be definitively the favored approach in any early stage EC and should be considered in selected advanced stages, especially in obese patients.
Disease prevention by a large population education on the deleterious effects of junk food and positive effects of physical activity along with the active treatment of installed obesity, are the best means to reduce the incidence and improve the prognosis of this increasingly frequent disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- PDQ Screening and Prevention Editorial Board In: PDQ Cancer Information Summaries [Internet]. National Cancer Institute (US); 2002-2016 Jun 30
- [Google Scholar]
- Survival of Danish patients with endometrial cancer in the intermediate-risk group not given postoperative radiotherapy: The Danish Endometrial Cancer Study (DEMCA) Int J Gynecol Cancer. 2011;21:1191-9.
- [Google Scholar]
- Menopausal hormone therapy and risk of endometrial carcinoma among postmenopausal women in the European Prospective Investigation Into Cancer and Nutrition. Am J Epidemiol. 2010;172:1394-403.
- [Google Scholar]
- Lifetime number of ovulatory cycles and risks of ovarian and endometrial cancer among postmenopausal women. Am J Epidemiol. 2016;183:800-14.
- [Google Scholar]
- The percentages of endometrial hyperplasia and endometrial cancer among polycystic ovary syndrome (PCOS) patients presenting with abnormal menstrual pattern. J Med Assoc Thai. 2014;97:159-64.
- [Google Scholar]
- Body mass index and mortality in endometrial cancer: A systematic review and meta-analysis. Gynecol Oncol. 2016;140:184-90.
- [Google Scholar]
- Etiologic heterogeneity in endometrial cancer: Evidence from a Gynecologic Oncology Group trial. Gynecol Oncol. 2013;129:277-84.
- [Google Scholar]
- Endometrial cancer and Lynch syndrome: Clinical and pathologic considerations. Cancer Control. 2009;16:14-22.
- [Google Scholar]
- Risks of colorectal and other cancers after endometrial cancer for women with Lynch syndrome. J Natl Cancer Inst. 2013;105:274-9.
- [Google Scholar]
- Lynch syndrome – Related endometrial carcinomas show a high frequency of nonendometrioid types and of high FIGO grade endometrioid types. Int J Surg Pathol. 2010;18:21-6.
- [Google Scholar]
- Global Database on Body Mass Index. WHO; 2016. Available from: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html
- Body fatness as a cause of cancer: Epidemiologic clues to biologic mechanisms. Endocr Relat Cancer. 2015;22:R125-34.
- [Google Scholar]
- Obesity, inflammatory markers, and endometrial cancer risk: A prospective case-control study. Endocr Relat Cancer. 2010;17:1007-19.
- [Google Scholar]
- Type I and II endometrial cancers: Have they different risk factors? J Clin Oncol. 2013;31:2607-18.
- [Google Scholar]
- Survival outcomes of obese patients in type II endometrial cancer: Defining the prognostic impact of increasing BMI. Gynecol Oncol. 2016;140:405-8.
- [Google Scholar]
- ESMO-ESGO-ESTRO Consensus Conference on Endometrial Cancer: Diagnosis, treatment and follow-up. Int J Gynecol Cancer. 2016;26:2-30.
- [Google Scholar]
- Is modified radical hysterectomy needed for patients with clinical stage I/II endometrial cancers? A historical control studyOncology. 2016;90:179-85.
- [Google Scholar]
- Salpingo-oophorectomy specimens for endometrial cancer staging: A comparative analysis of representative sampling versus whole tissue processing. Hum Pathol. 2013;44:643-50.
- [Google Scholar]
- Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane Database Syst Rev (09):CD006655.
- [Google Scholar]
- Laparoscopic-assisted vaginal hysterectomy versus total laparoscopic hysterectomy for the management of endometrial cancer: A randomized clinical trial. J Minim Invasive Gynecol. 2006;13:114-20.
- [Google Scholar]
- Hysterectomy in very obese and morbidly obese patients: a systematic review with cumulative analysis of comparative studies. Arch Gynecol Obstet. 2015;292(04):723-38. Oct doi: 10.1007/s00404-015-3680-7. Epub 2015 Mar 13
- [Google Scholar]
- Laparoscopy versus laparotomy for the management of endometrial carcinoma in morbidly obese patients: A prospective study. J Turk Ger Gynecol Assoc. 2015;16:164-9.
- [Google Scholar]
- Laparoscopic hysterectomy of large uteri with uterine artery coagulation at its origin. JSLS. 2008;12:25-9.
- [Google Scholar]
- Vaginal morcellation inside protective pouch: A safe strategy for uterine extration in cases of bulky endometrial cancers: Operative and oncological safety of the method. J Minim Invasive Gynecol. 2015;22:938-43.
- [Google Scholar]
- The use of MRI for selecting patients with endometrial cancer and significant co-morbidities for vaginal hysterectomy. Arch Gynecol Obstet. 2011;283:1097-101.
- [Google Scholar]
- Vaginal treatment of endometrial cancer: Role in the elderly. World J Surg Oncol. 2011;9:74.
- [Google Scholar]
- Lymphadenectomy for the management of endometrial cancer. Cochrane Database Syst Rev (09):CD007585.
- [Google Scholar]
- Intradermal radiocolloid and intraparenchymal blue dye injection optimize sentinel node identification in breast cancer patients. Ann Surg Oncol. 1999;6:450-4.
- [Google Scholar]
- Sentinel lymph node detection in endometrial cancer: Hysteroscopic peritumoral versus cervical injection. J Gynecol Oncol. 2016;27:e11.
- [Google Scholar]
- Detection rate and diagnostic accuracy of sentinel-node biopsy in early stage endometrial cancer: A prospective multicentre study (SENTI-ENDO) Lancet Oncol. 2011;12:469-76.
- [Google Scholar]
- Bilateral negative sentinel nodes accurately predict absence of lymph node metastasis in early cervical cancer: Results of the SENTICOL study. J Clin Oncol. 2011;29:1686-91.
- [Google Scholar]
- Sentinel Lymph node mapping in endometrial cancer: An update. Oncologist. 2016;21:461-6.
- [Google Scholar]
- The importance of applying a sentinel lymph node mapping algorithm in endometrial cancer staging: Beyond removal of blue nodes. Gynecol Oncol. 2012;125:531-5.
- [Google Scholar]
- Comparing indocyanine green, technetium, and blue dye for sentinel lymph node mapping in endometrial cancer. Gynecol Oncol. 2015;137:436-42.
- [Google Scholar]
- Factors associated with successful bilateral sentinel lymph node mapping in endometrial cancer. Gynecol Oncol. 2015;138:542-7.
- [Google Scholar]
- Prospective assessment of the prevalence of pelvic, paraaortic and high paraaortic lymph node metastasis in endometrial cancer. Gynecol Oncol. 2014;132:38-43.
- [Google Scholar]
- Predictive factor of conversion to laparotomy in minimally invasive surgical staging for endometrial cancer. Int J Gynecol Cancer. 2016;26:290-300.
- [Google Scholar]
- Technical development and results of left extraperitoneal laparoscopic paraaortic lymphadenectomy for cervical cancer. Gynecol Oncol. 2000;77:87-92.
- [Google Scholar]
- A comparison of extraperitoneal versus transperitoneal laparoscopic or robotic para-aortic lymphadenectomy for staging of endometrial carcinoma. Gynecol Oncol. 2014;132:366-71. et al. doi: 10.1016/j.ygyno.2013.12.019. Epub 2013 Dec 20.
- [Google Scholar]
- Minimally invasive comprehensive surgical staging for endometrial cancer: Robotics or laparoscopy? Gynecol Oncol. 2009;113:36-41. et al. doi: 10.1016/j.ygyno.2008.12.005. PMID: 19168206.
- [Google Scholar]
- Robotic infrarenal paraaortic and pelvic nodal staging for endometrial cancer: Feasibility and lymphatic complications. Acta Obstet Gynecol Scand. 2015;94:1074-81.
- [Google Scholar]
- A comparison of open surgery, robotic-assisted surgery and conventional laparoscopic surgery in the treatment of morbidly obese endometrial cancer patients. JSLS. 2015;19:e2014.00001.
- [Google Scholar]
- Robotic versus laparoscopic versus open surgery in morbidly obese endometrial cancer patients – A comparative analysis of total charges and complication rates. Gynecol Oncol. 2015;139:300-5.
- [Google Scholar]
- Medically inoperable endometrial cancer in patients with a high body mass index (BMI): Patterns of failure after 3-D image-based high dose rate (HDR) brachytherapy. Radiother Oncol. 2016;118:167-72.
- [Google Scholar]
- Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016;176:816-25.
- [Google Scholar]
- Obesity-related endometrial cancer: An update on survivorship approaches to reducing cardiovascular death. BJOG. 2016;123:293-8.
- [Google Scholar]
- Bariatric surgery decreases the risk of uterine malignancy. Gynecol Oncol. 2014;133:63-6.
- [Google Scholar]
- Hormone receptor expression patterns in the endometrium of asymptomatic morbidly obese women before and after bariatric surgery. Gynecol Oncol. 2014;133:78-82.
- [Google Scholar]







